Opioid Addiction And Treatment In Indiana
Opioid addiction has become one of the most serious health problems of our time, affecting families and communities across the nation. From prescription pain medications to illegal drugs like heroin and fentanyl, opioid use can lead to a dangerous addiction that feels nearly impossible to overcome.
While the journey to recovery from opioid addiction can be challenging, professional addiction treatment provides the medical care and therapeutic support needed to build a strong foundation for lasting recovery. At Indiana Center for Recovery, we work to provide a safe, supportive, and comfortable environment for healing. Through evidence-based treatments and personalized care plans, we are dedicated to providing the highest quality of care to those struggling with opioid addiction.
What are Opioids?
Opioids are a group of powerful drugs that work by attaching to special receptors in your brain and throughout your body. These receptors are mainly found in parts of the brain that control how you feel pain, emotions, and reward. This is why doctors use opioids to help manage pain – they’re very effective at blocking pain signals.
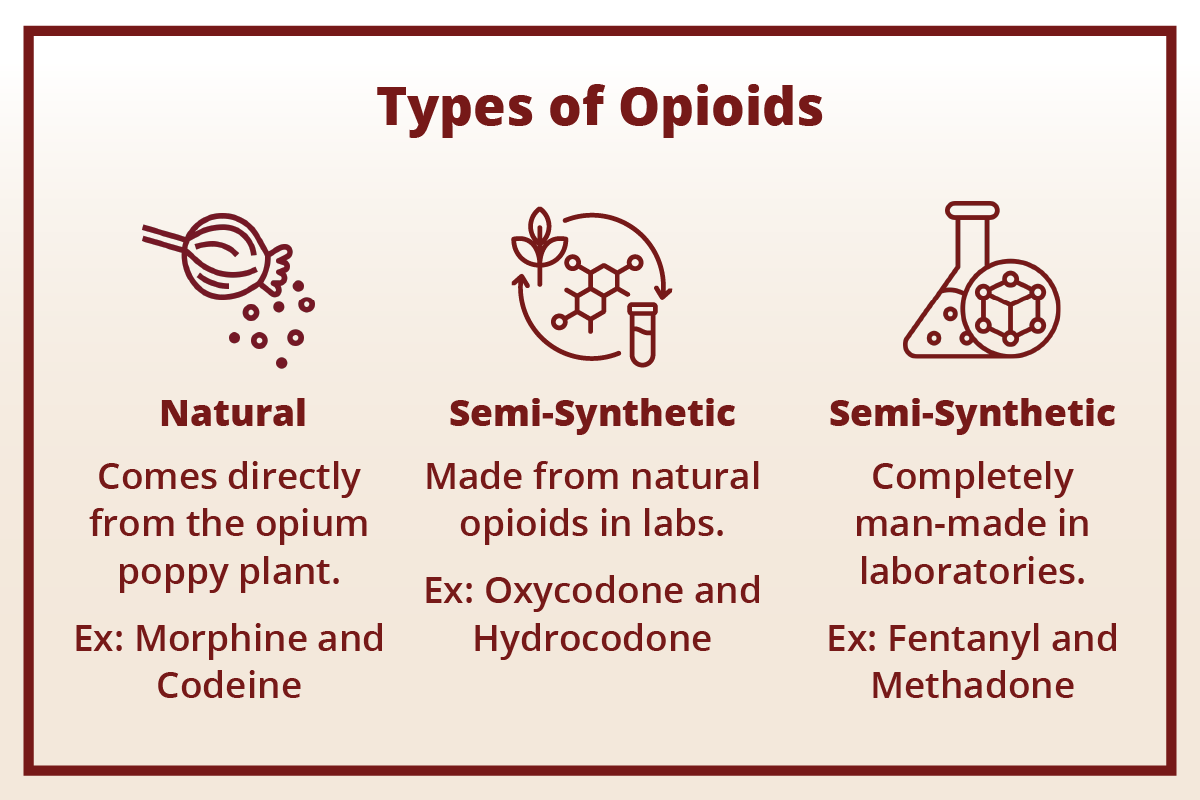
There are three main types of opioids:
- Natural opioids come directly from the opium poppy plant, like morphine and codeine.
- Semi-synthetic opioids are made from natural opioids in laboratories, such as oxycodone (OxyContin) and hydrocodone (Vicodin).
- Synthetic opioids are completely man-made in laboratories, including fentanyl and methadone.
Fentanyl deserves special attention because it has become increasingly common in recent years. This drug is extremely potent – up to 100 times stronger than morphine. Even tiny amounts can be deadly, which is why fentanyl-related overdoses have increased dramatically across the country.
Understanding Opioid Addiction
Understanding how opioid addiction happens can help remove shame and stigma. Addiction is not a moral failing or a lack of willpower – it’s a medical condition that changes how your brain works.
When you take opioids, they trigger the release of chemicals in your brain that make you feel good. Your brain remembers this feeling and wants to experience it again. Over time, your brain becomes dependent on the drug to feel normal. Tolerance develops when your body gets used to the drug, and you need more to get the same effect. Physical dependence means your body has adapted to the drug being present. If you stop taking it suddenly, you experience withdrawal symptoms. Addiction is when you continue using the drug despite harmful consequences to your life, relationships, work, or health.
What Can Cause Opioid Addiction
Multiple factors can contribute to someone developing an opioid addiction. Understanding these risk factors helps us approach addiction with compassion and treatment for opioid addiction.
Prescription Practices and Accessibility
Over-prescribing of opioids has been a major contributor to the addiction crisis. From the 1990s to early 2000s, opioid prescribing soared dramatically. By 2015, more than 1 in 3 U.S. adults received an opioid prescription. Even though prescribing has decreased by 44.4% in the past decade, many people who became dependent on prescription opioids have turned to illegal drugs when they can no longer access prescription medications ⓘ.
Easy access to opioids – whether through personal prescriptions, family medicine cabinets, or illegal sources – increases the risk of developing addiction. Studies show that more than 80% of people who use heroin started with prescription opioids ⓘ.

Genetics
Research shows that genetics play a significant role in addiction risk. Twin and family studies indicate that 23-54% of opioid addiction risk is inherited. This means that if you have family members with addiction, you may be at higher risk yourself ⓘ.
Scientists have identified several genes that may influence addiction risk, including variants in the OPRM1 gene (which affects how your body responds to opioids) and genes related to dopamine pathways in the brain. However, having these genetic variants doesn’t mean you will definitely develop addiction, it just means you may be more vulnerable ⓘ.
Check out how GeneSight can solve the issues of trial-and-error in finding the right medications for you in opioid addiction treatment.
Environmental and Psychosocial Factors
Your environment and life experiences significantly impact addiction risk, often more than genetics ⓘ. Important environmental factors include:
- Trauma and adverse childhood experiences like abuse, neglect, or witnessing violence can increase addiction risk. People often use substances to cope with emotional pain from past trauma.
- Mental health conditions such as depression, anxiety, PTSD, and antisocial personality disorder are strongly linked to higher rates of opioid addiction.
- Socioeconomic factors including poverty, unemployment, low education levels, and lack of access to healthcare increase vulnerability to addiction.
- Chronic pain conditions can lead to legitimate opioid use that sometimes develops into addiction, especially when pain is poorly managed through other means.
Social and Cultural Influences
The social environment around you plays a crucial role in addiction development:
Social isolation is both a cause and consequence of opioid addiction ⓘ. People who feel disconnected from others may use opioids to cope with loneliness, but opioid use often leads to further isolation from family and friends. Research shows that opioid users are more likely to have unstable social networks and tend to use alone, which increases overdose risk.
Cultural attitudes toward pain management and substance use in your community can influence addiction risk. Areas with lower social capital and community connectedness have higher rates of opioid overdoses.
Peer influence matters significantly. Associating with others who misuse opioids or other substances increases your risk of developing addiction.
Symptoms
Recognizing the signs and symptoms of opioid addiction is crucial for early intervention and effective treatment. Opioid addiction encompasses a range of physical, psychological, and behavioral manifestations that reflect the profound impact of opioids on the brain and body. While each individual may have their own experience, the following symptoms are indicative of opioid addiction and should be addressed:
Physical symptoms:
- Very small pupils (pinpoint pupils)
- Drowsiness or “nodding off”
- Slowed or shallow breathing
- Nausea and vomiting
- Severe constipation
- Weight loss or poor appetite
- Track marks or bruises from injection
- Wearing long sleeves to hide needle marks
Behavioral changes:
- Taking more medication than prescribed
- “Losing” prescriptions or asking for early refills
- Going to multiple doctors to get prescriptions (“doctor shopping”)
- Stealing medication from others
- Neglecting responsibilities at work, school, or home
- Withdrawing from family and friends
- Loss of interest in activities once enjoyed
- Risky behaviors to obtain drugs
Psychological symptoms:
- Intense cravings for opioids
- Inability to control use despite wanting to stop
- Mood swings, irritability, or anxiety
- Depression
- Paranoia or confusion
- Memory problems
Long-Term Effects of Opioid Addiction
As individuals continue to misuse opioids over an extended period, they are at risk of effects that can profoundly impact their quality of life and overall health. Prolonged opioid use takes a toll on the body, contributing to a range of physical health problems that can persist long after an individual stops using opioids.
Brain and nervous system changes:
- Permanent changes in brain structure and function
- Memory problems and difficulty concentrating
- Reduced ability to feel pleasure naturally
- Increased risk of depression and anxiety
Physical health problems:
- Respiratory depression and lung infections
- Heart problems, including irregular heartbeat and heart attacks
- Liver damage, especially when combined with alcohol
- Kidney problems
- Severe chronic constipation and bowel obstruction
- Increased risk of fractures and bone problems
- Compromised immune system, leading to frequent infections
Hormonal disruption:
- Decreased testosterone in men, leading to erectile dysfunction and infertility
- Menstrual irregularities and fertility problems in women
- Decreased bone density and osteoporosis
- Depression related to hormonal changes
Social and life consequences:
- Loss of relationships with family and friends
- Job loss and financial problems
- Legal troubles
- Homelessness
- Increased risk of overdose and death
For women specifically:
- Higher risk during pregnancy, including neonatal abstinence syndrome in babies
- Greater risk of polypharmacy (using multiple medications)
- Higher rates of accidental overdose
What are some forms of treatment for opioid addiction?
If you or a loved one is struggling with opioid addiction, it is important to seek professional help as soon as possible. At Indiana Center for Recovery, all patients undergo a thorough assessment of their condition to create a personalized plan that matches their needs for opioid addiction recovery. Treatment for opioid addiction includes detox, therapy, and medication management.
Detox
Detoxification, commonly referred to as detox, is often the first step in the treatment journey. The medical detox process involves the systematic removal of opioids from the body while managing withdrawal symptoms and ensuring the safety and comfort of the individual undergoing the process. This is always the first step in treatment, but detox alone is not enough for lasting recovery.
Medical supervision is essential because withdrawal can be uncomfortable and sometimes dangerous. At a medical detox facility, healthcare professionals:
- Monitor your vital signs 24/7
- Provide medications to ease withdrawal symptoms
- Ensure your safety and comfort
- Prepare you for the next phase of opioid abuse treatment
Withdrawal symptoms typically begin 12-30 hours after your last use and can include:
- Muscle aches and pains
- Nausea and vomiting
- Anxiety and restlessness
- Sweating and chills
- Sleep problems
- Strong cravings
Detox medications can make the process much more comfortable:
- Buprenorphine (Suboxone) reduces withdrawal symptoms and cravings
- Methadone helps manage severe withdrawal
- Clonidine reduces anxiety and other withdrawal symptoms
- Comfort medications for specific symptoms like nausea or sleep problems
The detox process typically lasts 5-7 days for most people, though it can vary based on individual factors.
Behavioral Therapy
Unlike detoxification, which focuses on managing the physical dependence on opioids, behavioral therapy addresses the psychological and emotional aspects of addiction. It helps you understand why you use drugs, learn healthy coping skills, and change behaviors that lead to drug use.
Cognitive Behavioral Therapy (CBT) is one of the most effective approaches. CBT helps you:
- Identify triggers that lead to drug use
- Challenge negative thoughts and beliefs
- Develop healthy coping strategies
- Build problem-solving skills
- Prevent relapse
Research shows that CBT is particularly effective for people who started with prescription opioids, helping them achieve longer periods of abstinence.
Other effective behavioral therapies include:
- Contingency Management – provides rewards for staying drug-free
- Motivational Interviewing – helps increase motivation to change
- Family Therapy – involves family members in the recovery process
- Group Therapy – provides peer support and shared experiences
Medication Management
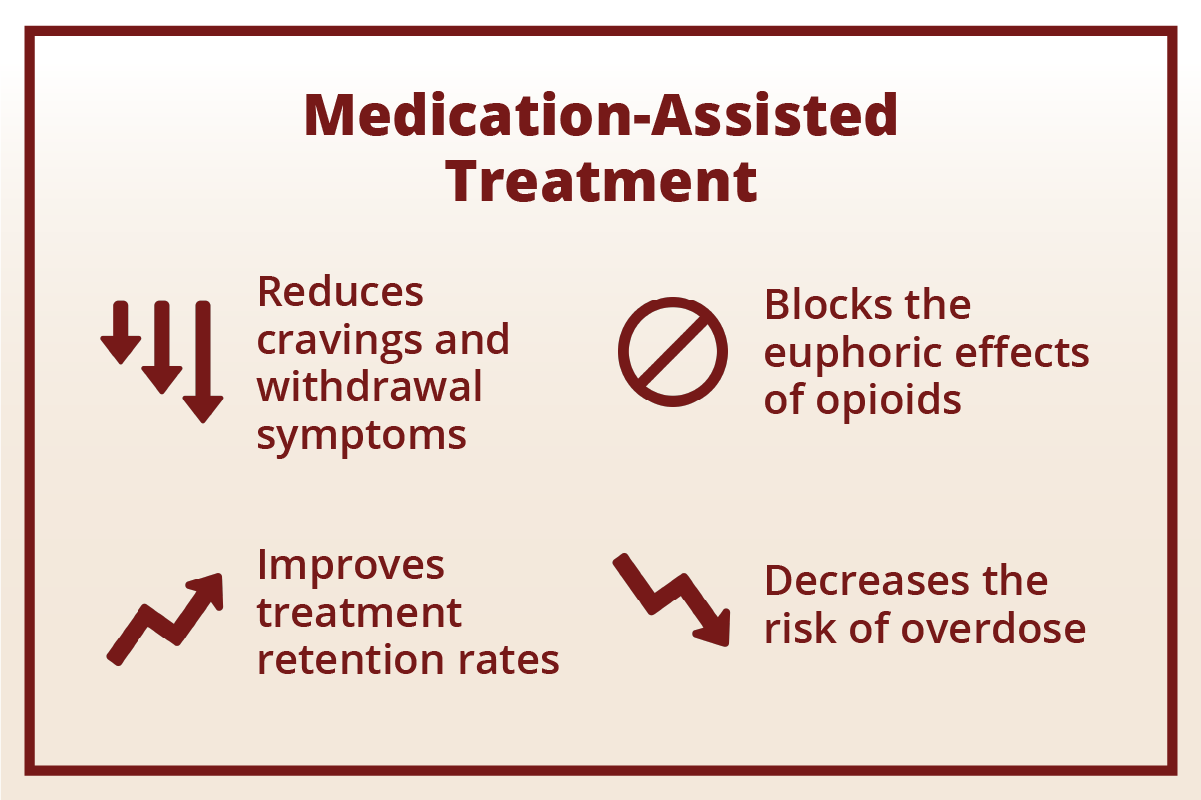
Medication-Assisted Treatment (MAT) combines FDA-approved medications with counseling and behavioral therapies. MAT is considered the gold standard for treating opioid addiction because it:
- Reduces cravings and withdrawal symptoms
- Blocks the euphoric effects of opioids
- Decreases the risk of overdose
- Improves treatment retention rates
The three main MAT medications are:
Methadone is a long-acting opioid that reduces cravings without causing a high. It must be dispensed daily from certified treatment programs.
Buprenorphine (often combined with naloxone in medications like Suboxone) reduces cravings and withdrawal with lower overdose risk. It can be prescribed by doctors in their offices.
Naltrexone (available as daily pills or monthly injections like Vivitrol) blocks opioid effects completely. It’s used after detox to prevent relapse.
These medications are not “trading one addiction for another”, they help normalize brain chemistry and allow people to focus on recovery without constant cravings.
How Long Is Rehab for Opioid Addiction?
The length of rehab for opioid addiction depends on several factors, including the severity of the addiction, any co-occurring mental or physical health conditions, and the specific needs and progress of the person in treatment.
Typical Duration of Rehab Programs
- Detoxification: The detox process often lasts 5-7 days, but some may need up to 10 days, especially if withdrawal symptoms are severe or if there are complications.
- Residential (Inpatient) Rehab: Most residential programs are about 30 days, but many people benefit from staying 60 to 90 days, or longer. The extended time allows for deeper recovery work and helps set up a solid foundation for sobriety.
- Intensive Outpatient Programs (IOP): IOP usually lasts 8-12 weeks, with patients attending treatment sessions several days per week.
- Standard Outpatient Treatment: This flexible option can last several months to a year or more, depending on individual needs. Sessions are less frequent, which is helpful for those balancing work or family responsibilities.
Individualized Treatment Timelines
Everyone’s recovery journey is different. Some may need longer periods in structured care to feel stable and confident in sobriety, while others may transition quicker to outpatient programs or aftercare support. The most successful outcomes come from a treatment plan tailored to a person’s unique needs, progress, and recovery goals.
Ongoing Recovery Support
Addiction is a chronic condition, so continuing care after formal rehab programs is crucial. Many people take part in aftercare services, counseling, or recovery groups for months or even years to maintain long-term recovery. The length of rehab is less important than getting the support you need for as long as you need it. Recovery is a lifelong journey, and seeking help is a courageous first step.
Levels of Care Available at Indiana Center for Recovery
At our facility, we are committed to providing comprehensive and individualized care to individuals seeking treatment for opioid addiction. In order to meet the unique needs of all our patients, we offer residential and outpatient treatment options. Our goal is to provide a continuum of care that addresses each individual’s unique challenges and strengths on their journey to recovery.
Residential
Our residential treatment program, also known as inpatient rehabilitation, provides 24-hour care in a safe, structured environment. Residential care provides a highly immersive and therapeutic experience that allows individuals to focus solely on their recovery journey without the distractions and stressors of daily life.
This level of care is ideal for people who:
- Have severe addiction requiring intensive medical supervision
- Need to be removed from triggers in their home environment
- Have tried outpatient treatment without success
- Have co-occurring mental health conditions
- Lack stable housing or strong family support
Residential treatment includes:
- Medical detoxification with 24/7 nursing care
- Individual and group therapy sessions
- Medication management
- Life skills training
- Family therapy and education
- Recreational and wellness activities
- Discharge planning and aftercare coordination
Our residential program typically lasts 30-90 days, depending on individual needs and progress. During this time, you’ll work closely with our medical team, therapists, and counselors to build a strong foundation for recovery.
Outpatient
Our outpatient programs offer a flexible and community-based approach to treating opioid addiction, providing individuals with the support and resources needed to navigate recovery while maintaining their daily responsibilities and routines. This level of care is ideal for those who do not require 24/7 medical supervision. We offer different levels of outpatient care:
Intensive Outpatient Program (IOP) provides 9-19 hours of treatment per week, including:
- Group therapy sessions
- Individual counseling
- Family therapy
- Medication management
- Educational workshops
- Relapse prevention planning
Outpatient Treatment (OP) involves 1-2 appointments per week with:
- Individual therapy sessions
- Medication management visits
- Periodic group therapy
- Case management services
- Crisis support when needed
Outpatient treatment works best for people who have:
- Completed residential treatment or medical detox
- Strong family and social support systems
- Stable housing
- Motivation to maintain recovery
- The ability to avoid triggers in their daily environment
All of our programs incorporate evidence-based treatments, including MAT, CBT, and other proven approaches. We work with you to create an individualized treatment plan that addresses your specific needs, circumstances, and goals.
Remember: Recovery is a journey, not a destination. At Indiana Center for Recovery, we’re here to support you every step of the way. Whether you need intensive residential care or flexible outpatient services, we have the expertise and compassion to help you achieve lasting recovery.
If you or a loved one is struggling with opioid addiction, don’t wait to get help. Contact Indiana Center for Recovery today for to learn how we can help you begin your journey toward a healthy, fulfilling life in recovery. You are worth it, and recovery is possible.
Opioid Addiction Treatment at Indiana Center For Recovery
If you’re struggling with opioid addiction, professional treatment can help you overcome dependency and rebuild your life. At Indiana Center for Recovery, we provide comprehensive addiction treatment programs that begin with medical detox programs to safely manage opioid withdrawal symptoms, which can be severe without medical supervision. Following detox, intensive inpatient rehab provides round-the-clock support for recovery, while flexible outpatient treatment options allow you to maintain daily responsibilities while receiving ongoing care. Opioid addiction often co-occurs with mental health conditions, our integrated dual diagnosis treatment addresses both addiction and mental health simultaneously.
We offer rehab centers across Indiana where you can access specialized opioid addiction treatment programs with medically supervised detox and comprehensive care. Call us right now at (844) 650-0064 to learn how we can help you overcome opioid addiction and start your journey toward recovery.



 100% Confidential
100% Confidential