BPD vs. Bipolar Disorder: Why Knowing The Difference Matters
Clinically Reviewed by:
Living with intense mood swings is hard enough. Getting the wrong diagnosis can make it even harder. Borderline Personality Disorder (BPD) and Bipolar Disorder share some symptoms, yet they are two separate conditions that need different care. Understanding where they overlap, and where they don’t can guide you or a loved one toward the right help and better recovery.
Understanding BPD and Bipolar Disorder
Borderline Personality Disorder (BPD) and Bipolar Disorder are two mental health conditions that can look similar but are actually quite different.
Borderline Personality Disorder (BPD)
BPD is a personality disorder that affects how a person thinks and feels about themselves and others. People with BPD often have intense emotions, unstable relationships, and a shaky sense of self.
- A long-term pattern of unstable emotions, self-image, and relationships.
- Feelings can flip in minutes or hours, often triggered by fear of abandonment or conflict.
- About 1.4% of U.S. adults live with BPD.
Bipolar Disorder
Bipolar Disorder is a mood disorder. It causes extreme mood swings, including emotional highs (mania or hypomania) and lows (depression). These mood episodes can last for days, weeks, or even months.
- A mood disorder marked by distinct “episodes” of mania/hypomania (high energy) and depression (low energy).
- Episodes last days to weeks and come with changes in sleep, activity, and thinking.
- Roughly 2.8% of Americans are affected.
Shared Symptoms of Bipolar Disorder and BPD
BPD and bipolar disorder share some symptoms, which is why they are sometimes confused. Common overlapping symptoms include:
- Mood swings: Both conditions can cause rapid changes in mood.
- Impulsivity: Acting without thinking, sometimes in risky ways.
- Irritability or anger: Both can lead to sudden outbursts.
- Depression: Feelings of sadness, hopelessness, or emptiness.
- Self-destructive behaviors: Such as substance abuse or self-harm.
Despite these similarities, the reasons behind these symptoms and how they appear can be quite different.
The Dangers of Misdiagnosis
Because BPD and bipolar disorder share symptoms, misdiagnosis is common. This can be dangerous because:
Wrong treatment
Bipolar disorder is usually treated with medication, while BPD is best treated with therapy. The wrong treatment can make symptoms worse or delay recovery.
One example is giving antidepressants alone to someone with an undiagnosed bipolar disorder, which can trigger mania or rapid cycling.
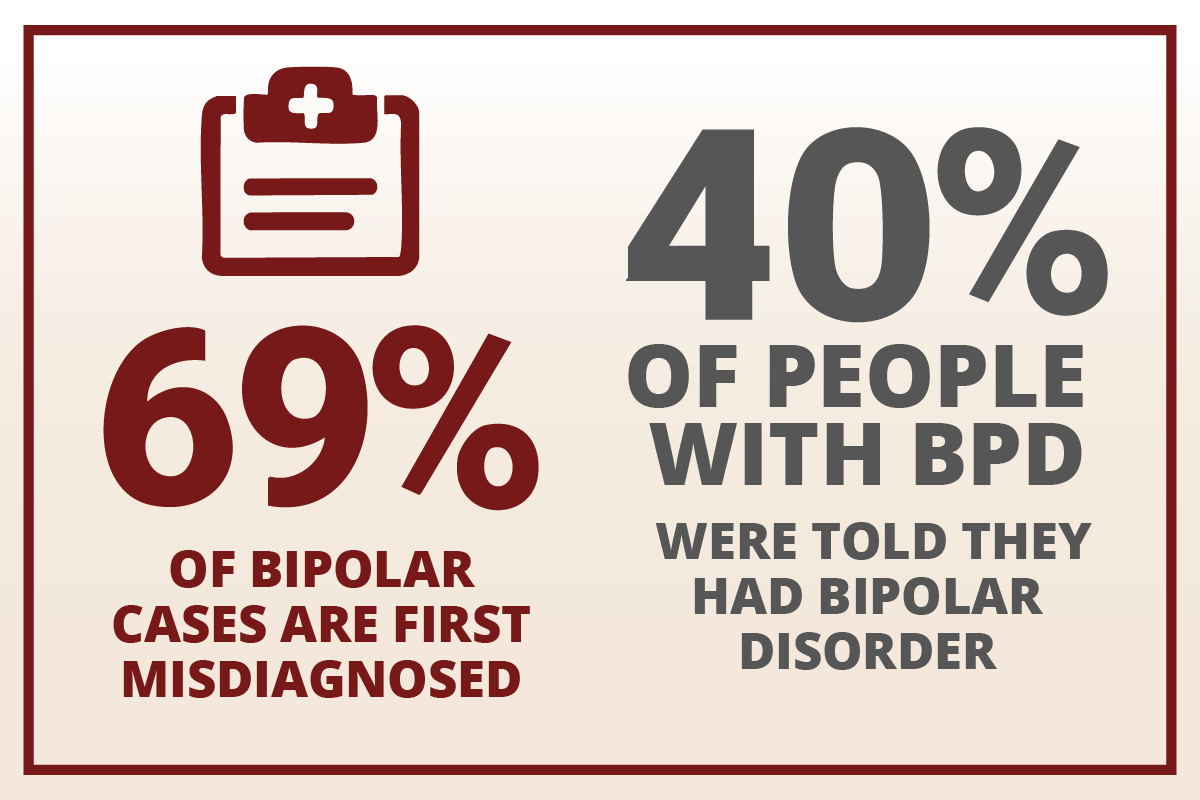
About 69% of people who truly have bipolar disorder are first misdiagnosed, often with unipolar depression, delaying proper treatment by years.
Increased risk
Misdiagnosis can lead to higher risks of self-harm or suicide, especially if symptoms are not managed properly. One in ten people with BPD die by suicide, and up to 70% attempt it at least once.
Emotional impact
Not knowing your true diagnosis can be confusing and discouraging. Nearly 40% of people with BPD report being told they had bipolar disorder at some point.
Accurate diagnosis by a mental health professional is essential for effective treatment and better outcomes.
BPD vs. Bipolar: Key Differences
| Feature | BPD | Bipolar Disorder |
| Type | Personality disorder | Mood disorder |
| Mood Swings | Rapid, often triggered by events (hours to days) | Last longer (days to months), not always triggered by events |
| Self-Image | Unstable, changes frequently
| Usually stable outside of mood episodes |
| Relationships | Intense, unstable, fear of abandonment
| Not a defining feature |
| Impulsivity | Common, often in response to emotions | Can occur during mania or depression |
| Treatment | Mainly therapy (DBT, CBT), some medications | Medications (mood stabilizers, antipsychotics), therapy |
Understanding the Nature of Each Condition
Borderline Personality Disorder is classified as a personality disorder, which means it affects how a person consistently thinks, feels, and behaves in relationships and daily life. Bipolar disorder, on the other hand, is a mood disorder that primarily affects a person’s emotional states and energy levels in distinct episodes.
How Mood Swings Present Differently
People with BPD experience rapid mood changes that typically last hours to a few days and are often triggered by specific events or interactions, especially in relationships. In contrast, bipolar disorder involves longer mood episodes that can persist for days, weeks, or even months, and these episodes may occur without any clear external trigger.
Self-Image and Identity Patterns
Individuals with BPD frequently struggle with an unstable sense of self that can change dramatically based on circumstances or relationships.
Their self-image may shift from feeling worthless to feeling important, sometimes within the same day.
People with bipolar disorder generally maintain a more stable sense of identity, though their self-esteem may fluctuate during mood episodes.
Relationship Dynamics
BPD significantly impacts how people form and maintain relationships, often creating intense, unstable connections marked by a deep fear of abandonment.
These relationship patterns are a core feature of the disorder. While bipolar disorder can affect relationships during mood episodes, unstable relationship patterns are not a defining characteristic of the condition.
Impulsive Behaviors
Both conditions can involve impulsive actions, but they stem from different sources. In BPD, impulsivity often occurs as an immediate response to intense emotions or relationship conflicts. In bipolar disorder, impulsive behaviors typically happen during specific mood episodes, particularly during manic or hypomanic states.
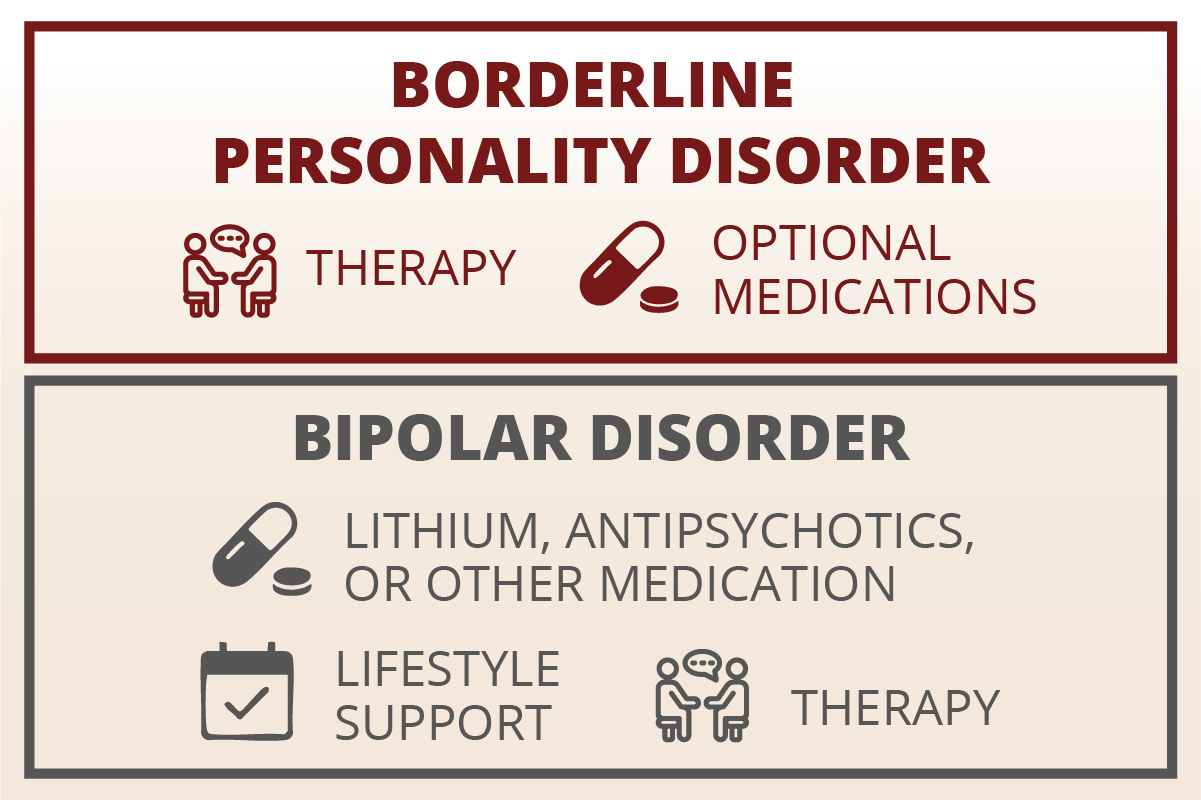
Treatment Approaches
The primary treatment for BPD centers on specialized therapy, particularly Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT), with medications used as supplements for specific symptoms.
Bipolar disorder treatment relies heavily on medications such as mood stabilizers and antipsychotics as the foundation, with therapy serving as an important but secondary support tool.
Remember: Both conditions can exist together. A thorough assessment may involve several appointments, mood tracking, and input from family or partners.
Treatment Options for BPD and Bipolar Disorder
Treatment for BPD
Dialectical Behavior Therapy (DBT) serves as the primary treatment approach for Borderline Personality Disorder. This specialized therapy teaches essential skills in four key areas: mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. Clinical trials have demonstrated that DBT significantly reduces self-harm behaviors and emergency room visits, with these positive benefits lasting up to two years after treatment completion.
Other effective therapeutic approaches include Mentalization-Based Treatment (MBT) and schema therapy, though these may have more limited availability in some areas. While medications are not considered the main treatment for BPD, they may be prescribed to target specific symptoms such as anxiety or depression that commonly occur alongside the disorder.
Treatment for Bipolar Disorder
Medication forms the foundation of bipolar disorder treatment. Mood stabilizers such as lithium and valproate are commonly prescribed, along with atypical antipsychotics. Antidepressants may sometimes be included in the treatment plan, but they are typically paired with a mood stabilizer to prevent triggering manic episodes.
Psychotherapy plays a crucial supporting role in bipolar disorder treatment. Cognitive Behavioral Therapy (CBT) helps patients develop better coping strategies and recognize early warning signs of mood episodes. Family-focused therapy involves loved ones in the treatment process, while psychoeducation programs help both patients and families understand the condition better. These therapeutic approaches significantly improve medication adherence and overall treatment outcomes.
Lifestyle supports are equally important in managing bipolar disorder. Maintaining a regular sleep schedule helps prevent mood episodes, as sleep disruption is a common trigger. Limiting alcohol and drug use is essential, as these substances can interfere with medications and worsen symptoms. Developing effective stress-management strategies helps individuals cope with daily challenges without triggering mood episodes.
GeneSight Testing: A Personalized Approach to Medication
While there’s no genetic test that can diagnose bipolar disorder, GeneSight can help doctors choose the right medication after a diagnosis is made.
What it does
GeneSight uses a quick cheek swab to look at how your body’s genes affect the way you respond to common mental health medications like mood stabilizers, antidepressants, and antipsychotics. The results help doctors understand which medications may work better for you and which ones might cause more side effects.
Why it matters
Finding the right medication for bipolar disorder can take time. GeneSight testing helps reduce some of the trial-and-error by showing how your body may react to certain drugs. This can lead to fewer side effects and a quicker path to feeling better.
Important to know
GeneSight doesn’t diagnose bipolar disorder. It’s a tool to help guide treatment once a diagnosis has been made. Your doctor will still consider your full medical history, symptoms, and other factors when creating a treatment plan.
Shared Support Strategies
Crisis planning is vital for both conditions and involves creating a detailed plan for managing emergency situations. This includes having 24/7 resources readily available, such as the 988 Suicide & Crisis Lifeline, which can be reached by calling or texting 988 in the United States for immediate support during suicidal thoughts or crisis situations.
Involving loved ones in therapy sessions can build understanding and reduce stigma surrounding both conditions. Family members and close friends learn how to provide appropriate support while maintaining healthy boundaries. This collaborative approach often leads to stronger relationships and better treatment outcomes.
Joining peer-support groups provides valuable connection with others who understand the challenges of living with these conditions. These groups help reduce feelings of isolation and provide practical advice from people with lived experience. Many find that sharing their stories and hearing from others creates a sense of community and hope for recovery.
Get Help Today
If you recognize these symptoms in yourself or someone you care about, know that hope and effective help exist. Clear diagnosis opens the door to targeted treatment, whether that is Dialectical Behavior Therapy (DBT) skills for BPD or mood-stabilizing medication for bipolar disorder. With the right plan, people move from crisis to stability, rebuild relationships, and reclaim their futures. If uncertainty remains, call the Indiana Center for Recovery for a comprehensive assessment. Our mental health professionals are experienced in diagnosis and treatment of both Borderline Personality and Bipolar Disorder.






 100% Confidential
100% Confidential